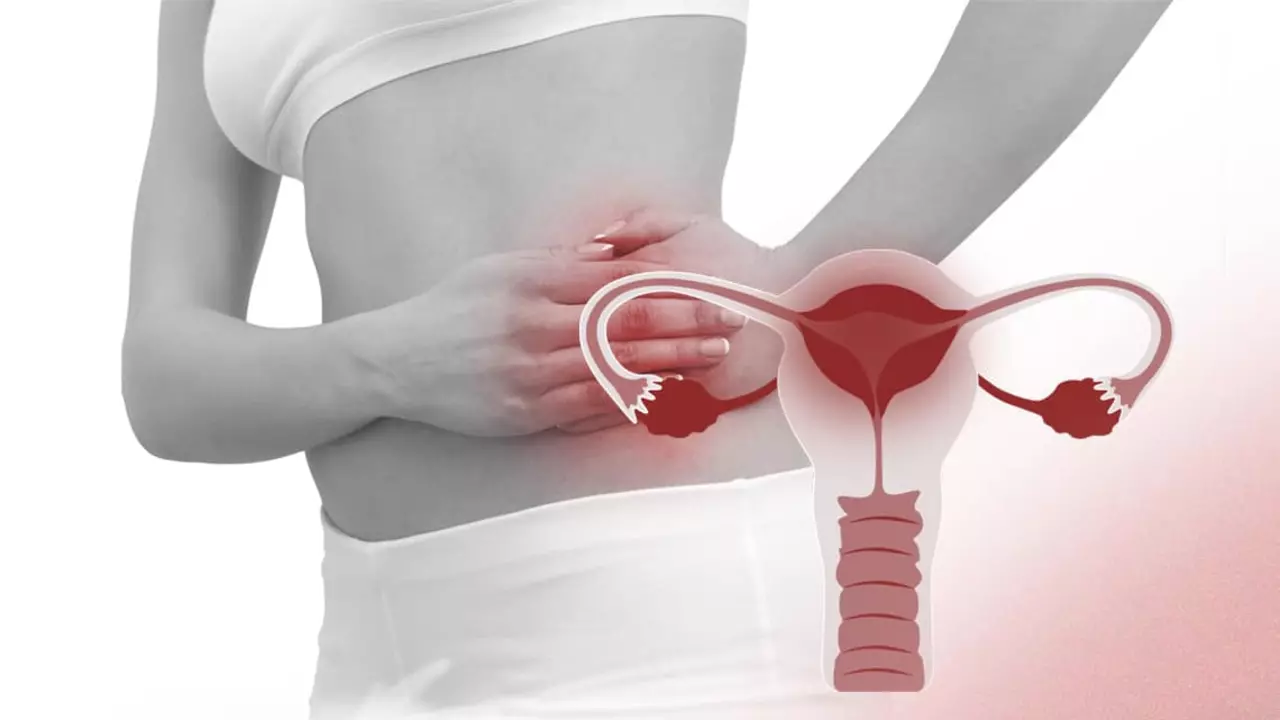
Pelvic congestion syndrome (PCS) is a condition that primarily affects women and is characterized by chronic pelvic pain. The pain is often associated with the presence of varicose veins in the pelvis, resulting from blood flow issues in the pelvic veins. It’s a condition that can easily be overlooked and is sometimes misdiagnosed since its symptoms can mirror those of other conditions. Weight gain is not commonly listed as a direct symptom of PCS, but the condition can be associated with feelings of heaviness and bloating in the pelvic area, which might be mistaken for an increase in weight.
Understanding PCS and its impact on a person’s body is essential for proper diagnosis and management. While the syndrome itself is not a direct cause of weight gain, the chronic pain and discomfort it brings can potentially lead to a decrease in physical activity. This reduction in physical activity could, in some cases, contribute indirectly to weight changes. Women experiencing symptoms of PCS should consult with their healthcare provider for an accurate diagnosis and appropriate treatment.
Reader's Roadmap
Key Takeaways
- Pelvic congestion syndrome is a chronic condition causing pelvic pain but does not directly cause weight gain.
- Misinterpretation of PCS symptoms like bloating can lead to the misconception of weight gain.
- Reduced activity due to PCS pain may indirectly influence weight.
Understanding Pelvic Congestion Syndrome
Pelvic congestion syndrome (PCS) often leaves many dealing with challenging symptoms, while the underlying causes are closely linked to vascular issues and hormonal influences.
Symptoms and Causes
PCS manifests through chronic pain in the pelvic or abdominal area. This discomfort is due to issues with the pelvic veins, specifically when varicose veins develop in this region, similar to those that can appear in the legs. People with PCS might experience a dull, aching sensation that intensifies after standing for long periods or during sexual intercourse. Here’s a quick breakdown of the causes:
- Faulty Valves: The valves in the ovarian vein may not function properly, leading to blood pooling.
- Pressure: Pregnancy or pelvic tumors can increase pressure on pelvic veins, exacerbating symptoms.
- Hormonal Changes: Fluctuating levels of estrogen may weaken the vein walls.
Role of Estrogen and Venous System
Estrogen and the venous system play pivotal roles in PCS:
- Estrogen Impact: This hormone is thought to weaken vein walls, which could contribute to varicose veins in the pelvic area.
- Venous Inefficiency: Inefficient blood flow caused by venous issues is a hallmark of PCS. The pelvic veins become enlarged because of the impaired blood flow, and the valves inside the veins may fail to keep blood moving correctly, leading to congestion.
Pelvic congestion syndrome can be a perplexing and distressing condition, but understanding the symptoms and roles of both estrogen and the venous system can demystify it and support individuals on their journey to relief.
Diagnosis and Imaging Techniques
When it comes to understanding pelvic congestion syndrome (PCS), doctors have a variety of tools at their disposal, from basic tests to sophisticated imaging. Let’s take a look at how these methods can help unravel the complexities of PCS diagnosis.
Common Diagnostic Tests
For anyone suspecting PCS, initial diagnosis typically begins with a pelvic ultrasound. It’s a non-invasive test that uses sound waves to create images of structures within the pelvis. This test can help identify enlarged veins that might suggest PCS. Additionally, venography, which involves injecting a contrast dye into the pelvic veins to make them visible on X-ray images, can also be used. In venography, doctors look for the backward flow of blood, or reflux, which is indicative of PCS.
Advanced Imaging Options
To further investigate PCS, more advanced imaging may be required. Magnetic resonance imaging (MRI) provides a more detailed image and can be particularly effective in examining the pelvic veins and surrounding structures. MRI is advantageous because it doesn’t use ionizing radiation and offers a comprehensive view of the pelvic anatomy.
Alternatively, a computed tomography (CT scan) can also provide cross-sectional images of the body and may assist in ruling out other causes of pelvic pain. What sets MRI and CT apart is their ability to give a crystal-clear picture of internal structures, helping to paint a full picture for an accurate diagnosis.
Treatment Strategies

When it comes to managing Pelvic Congestion Syndrome (PCS), the focus is on alleviating the chronic pain and discomfort it causes. The treatment strategies for PCS typically revolve around two main approaches: medications and hormonal therapy, and surgical interventions, each targeting the underlying issues of the condition.
Medications and Hormones
Patients with PCS are often prescribed a variety of medications aimed at managing symptoms and improving vein health. Medications such as pain relievers can reduce the discomfort associated with the condition. For hormonal regulation, doctors may prescribe oral contraceptives or medroxyprogesterone acetate which work by decreasing blood flow to the veins in the pelvic region, thus reducing pain and swelling.
- Gonadotropin-releasing hormone agonists are another pharmacological treatment, used to reduce estrogen levels and alleviate symptoms of PCS.
List of commonly used medications:
- Pain medications: for symptom relief
- Oral contraceptives: to regulate menstrual cycle and reduce pelvic congestion
- Danazol: an option to suppress ovulation and menstrual flow
- Medroxyprogesterone acetate: helps in reducing menstrual flow and pelvic congestion
- Gonadotropin-releasing hormone agonists: reduces estrogen, which may be contributing to vein dilation
Surgical Interventions
In cases where medications are not effective, surgical interventions may be recommended. The primary surgical treatment for PCS is embolization, a minimally invasive procedure where a catheter is used to introduce agents that close off faulty veins.
- Ovarian vein embolization specifically targets the ovarian vein where a sclerosing agent is introduced to seal the vein, preventing blood from pooling.
Laparoscopy and hysterectomy are other surgical options, with the former being less invasive and the latter considered in more severe cases or when other conditions are present.
Options under surgical interventions include:
- Vein embolization: Blocking the abnormal veins to reduce congestion
- Sclerotherapy: Injection of sclerosing agents to collapse problematic veins
- Laparoscopy: A minimally invasive surgery to address pelvic veins
- Hysterectomy: Removal of the uterus, considered when other treatments fail and patient is not planning future pregnancies
In conclusion, treating Pelvic Congestion Syndrome is a matter of combining effective pain management with procedures that address the venous insufficiency at the core of the condition. Understanding these options allows individuals to consult with their healthcare providers to determine the most appropriate treatment for their specific situation.
Living with Pelvic Congestion Syndrome

Pelvic Congestion Syndrome (PCS) is a condition that primarily affects women in their reproductive years, leading to chronic pelvic pain which can continue even after reaching menopause. It’s a bit like having varicose veins, but in the pelvic area. This pain can be particularly intense during the menstrual cycle and can interfere with regular activities and overall well-being.
Those living with PCS may find sexual intercourse painful, and activities that put pressure on the pelvic area, such as sitting or standing for long periods, may exacerbate discomfort. It’s not uncommon to experience a feeling of bloating or heaviness as well.
Pain Management
- Medication: Over-the-counter pain relievers or prescribed medications can help manage symptoms.
- Physical Therapy: Certain exercises can alleviate the pain.
- Lifestyle Adjustments: Taking regular breaks to lie down and elevate the legs can provide relief.
Lifestyle Adjustments
- Exercise: Regular, gentle exercise, like swimming or walking, can improve blood flow and decrease pain.
- Diet: A well-balanced diet helps maintain proper weight, potentially reducing symptoms.
- Support: Wearing compression stockings might help by supporting the veins.
People with PCS can also face a psychological impact due to chronic pain, which might affect their mood and lead to feelings of frustration or sadness. Support groups and counseling can play an integral role in coping with these emotional challenges.
Regarding whether PCS causes weight gain – it’s not directly responsible. However, bloating associated with PCS may give the sensation of weight gain, and the pain might limit physical activity, which can indirectly affect weight. It’s important to consult with healthcare providers for a comprehensive treatment plan that addresses both physical and emotional aspects.